Definition
Seizure : abnormal neural discharge in the cerebral cortex that result in abnormal function, the nature of clinical manifestations depends on the regions of the brain affected.
Epilepsy : Recurrent seizures unrelated to fever or acute cerebral insult.
Epilepsy- questions ?
- 1- seizure?
- 2- seizure-type?
- 3- fits a syndrome?
- 4- identifiable cause?
- 5- anti-epileptic drug (AED)?
- 6- when to stop treatment?
- 7- surgery?
History of events
- Frequency
- Timing
- Duration * Triggers
- Warning
- Color change- pallor, cyanosis
- Alteration in consciousness
- Motor phenomena
- Associated s/s- incontinence, injury
- Symptoms following attack- postictal
Differential diagnosis
- Pseudo seizure- psychiatric
- Syncope- cardiac or neurological
- Movement disorder
- Migraine
- Transient ischemic attack
- Metabolic disorders- hypoglycemia
- Anoxia/hypoxia
Epilepsy: Classification
Generalized tonic clonic seizures
• Main seizure type: In -10% epileptics
• Tonic phase:
- Stiff, crying out, tongue bite, apnea, cyanosed
- Increase heart rate, blood pressure
- Fall, labored breathing, salivation
• Clonic phase:
- Intermittent clonic movements of muscles
- Brief relaxations, involves all limbs
- Incontinence at the end of clonic phase, lasts for few minutes
• Post-ictal period:
Drowsiness, confusion, headache, deep sleep
Causes of Epilepsy
- Idiopathic: 72%
- Can be determined: 28% case
Determined causes:
- Inherited genetic:
- Acquired :Trauma, Neuro surgery. Inflammatory, Metabolic, Infections, Tumor, Toxic disorders, drugs
- Congenital: Inborn error of metabolism.
- Withdrawal of drugs:
- Congenital: Inborn error of metabolism.
- Withdrawal of drugs:
Alcohol
Barbiturates
Anti-Epileptics
Benzodiazepines
Management
- First priorities:
- Attention to vital signs
- Respiratory and cardiovascular support
- Treatment of seizures if they resume
- To be followed by:
Management of life-threatening conditions CNS infection, metabolic derangement and drug toxicity
- When the patient is not acutely ill:
Evaluation should initially focus on whether there is a history of earlier seizures
Anti Epileptic Drugs (AED) Classification
- Older AEDs:
- Phenobarbital, Phenytoin, Primidone
- Ethosuximide , Carbamazepine , Valporate
- Newer AEDs:
- Lamotrigine, Topiramate, Tiagabine
- Oxcarbazepine, Zonisamide, Levetiracetam
- Vigabatrin, Felbamate, Pregabalin
- Rufinamide, Lacosamide, Stiripentol, Clobazam
- Eslicarbazepine, Ezogabine, Perampanel
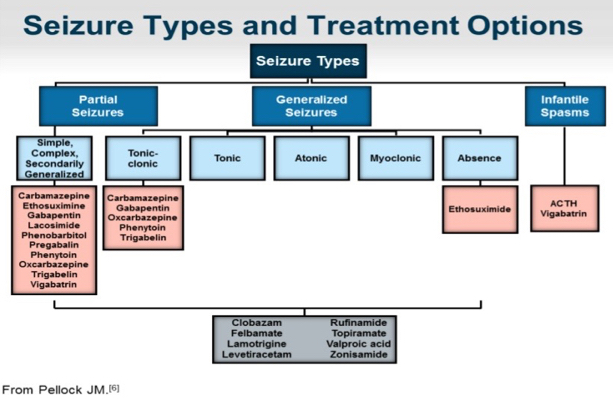
Seizure: Types and choice of AEDs
Facilitation of GABA mediated Chloride channel opening
• Barbiturate
• Benzodiazepine
• Vigabatrin
• Valproate
• Gabapentin
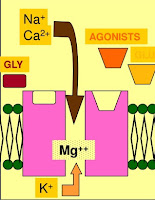
Glutaminergic synapse
Magnesium ions in resting state
- Enhancement:
Glycine (GLY) binding enhances the ability of GLU or NMDA to open the channel
- Agonists:
NMDA, AMPA, Kianate
Ethosuximide
• Mechanism of action:
- It has an important effect on Ca 2+ currents, reducing the low-threshold (T-type) current.
• Pharmacokinetics:
- t1/2 :40 hours
- Metabolism: Hydroxylation inactive products
• Adverse reactions:
- Gastric distress including pain, nausea, and vomiting
• Dose: 20-30mg/kg/day